Study published in Hypertension reveals significant findings regarding hormone replacement therapy (HRT) and cardiovascular health
According to a recent study published in the peer-reviewed American Heart Association journal, Hypertension, women taking oral estrogen hormones for hormone replacement therapy (HRT) may face a higher risk of developing high blood pressure compared to those using non-oral forms of HRT. The study, funded by the Canadian Institutes of Health Research, analyzed data from over 100,000 women aged 45 years and older who were prescribed estrogen-only hormone therapy in Alberta, Canada, between 2008 and 2019.
The study’s most notable finding is that the use of non-oral estradiol, a specific form of estrogen, at the lowest dose and for the shortest duration, was associated with the lowest risk of developing high blood pressure. In comparison, oral estrogen was found to increase the risk of high blood pressure by 14% compared to transdermal cream and by 19% compared to vaginal estrogen creams or suppositories. Additionally, the study highlighted that longer-term use of estrogen or higher dosage further heightened the risk of high blood pressure.
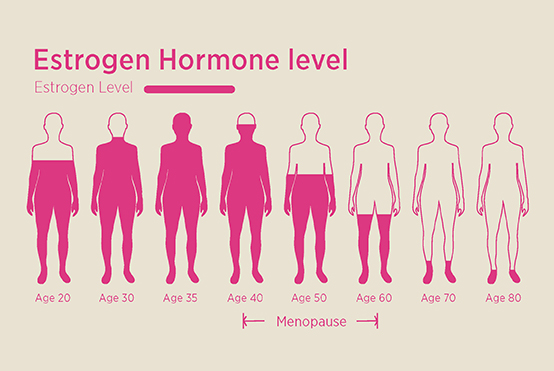
These findings suggest that different types of estrogen may carry varying cardiovascular risks for women undergoing hormone replacement therapy during menopause. The study authors emphasize the importance of considering safer alternatives to oral estrogen for HRT.
Experts in the field have expressed their views on the research, emphasizing the impact of estrogen on blood vessels. Dr. Jennifer Bourgeois, a pharmacy and health expert, points out that while estrogen’s cardioprotective effects on vascular inflammation are well-established, its role in hypertension remains debatable. The study findings align with previous evidence that non-oral HRT preparations, particularly transdermal estrogen, are safer options with lower risks of venous thromboembolism. A systematic review published in the Archives of Gynaecology and Obstetrics confirms the clinical difference between administration routes, favoring transdermal HRT over oral administration.
Dr. Zahra Ameen, a consultant gynecologist and obstetrician, explains that transdermal HRT preparations are as effective as oral preparations in alleviating HRT symptoms. Furthermore, the lower doses required for transdermal preparations produce equivalent benefits due to the avoidance of liver metabolism. It is worth noting that estrogen prescribed as a gel or patch widens blood vessels, aiding in blood pressure reduction.
The study has certain limitations, as it only focused on women over 45 years of age using estrogen-only therapy. Dr. Ameen emphasizes the need for further research, particularly in the context of combined HRT preparations containing both estrogen and progesterone. Micronized progesterone, commonly used in such combinations, has shown no significant effect on blood pressure and can even help to lower it.
Before initiating HRT, it is crucial to assess individual risk factors for blood pressure elevation, such as age, general health, weight, smoking status, and the presence of an intact uterus. A careful risk-benefit analysis should be conducted, considering the potential improvement in quality of life offered by HRT.
Maintaining a healthy lifestyle is paramount for managing blood pressure during menopause, regardless of HRT usage. Health experts recommend following a heart-healthy diet, reducing caffeine intake, quitting smoking, engaging in regular exercise, and managing stress. A comprehensive approach to postmenopausal health includes these lifestyle factors to reduce the risks of stroke, high blood pressure, and cardiovascular disease.
In light of this research, it becomes increasingly important for women and healthcare providers to consider safer alternatives to oral estrogen hormones in hormone replacement therapy, prioritizing cardiovascular health during menopause and beyond.